There are two very distinct types of leg ulcer:
Non-healing injury or surgical wound on healthy legs
Often from a knock to the shin, patients can end up in a cycle of going to the NHS for redressings twice a week for months and even years. The dressings typically used make the wound too wet especially if honey is used. The dressings put pressure in the wound. The wounds are often cleaned aggressively twice a week. Any of which is enough to stop the wound healing.
Using the podiatry wound care technique we can usually heal this type with 3 or 4 appointments. You can find some testimonials of this from previous patients at the end of this page.
Non-healing wound on an unhealthy leg
This can still start with a knock or it can come on its own. The skin on an unhealthy leg usually looks abnormal, it could be related to fluid swelling or a blood circulation issue. The skin can be either sclerotic (hard), red or brown stained, with flaky or silvery skin, swollen with or without leaking fluid.
These are much harder to treat, it would take longer and we might not be able to offer anything in addition to what is available from the NHS. That said patients who come usually report increased comfort and they tend to have a decreased number of infections and increased healing, though still slow.
There is also an increasing number of patients with very chronic wounds who have been told to treat it themselves as there is a shortage of NHS staff, in which case we're here for you if you need us.
If you are unsure which applies to you get in touch and we can advise you.
Why you should see a podiatrist for your leg wound
Even your GP might not know this but Podiatrists are the specialists for lower limbs up to the hip - not just feet.
Also because of the prevalence of diabetic foot ulcers podiatrists are the only medical professionals that are trained in ulcer care during their initial training. Of course how to apply various types of dressings but also understanding the physiology of wound healing, how to provide pressure relief and sharp debridement, which is removing debris that can block healing. Not all podiatrists but many like Mr Thomson have had further experience treating ulcers while working in the NHS.
The well proven principles that podiatrists use for diabetic foot ulcers work supremely well on all other areas of skin too: Protection from damage and infection. Pressure relief. Fluid drainage. Avoiding contamination by keeping it from getting wet while bathing. We add as little as possible into wounds, ideally nothing directly in the wound other than temporarily for very specific reasons. Instead we use simple dressings and padding to create an ideal environment for the body to get on with healing the wound. Not too wet and not too dry.
The podiatry method is impossible without scalpel use. Other professions rely on keeping wounds wet to have a chance of removing debris from the wound. It is perhaps counter intuitive but it is much gentler to use a scalpel than rubbing with gauze or pads. It also allows the wound to dry out and heal.
The podiatry difference on non-healing leg injuries and surgical wounds
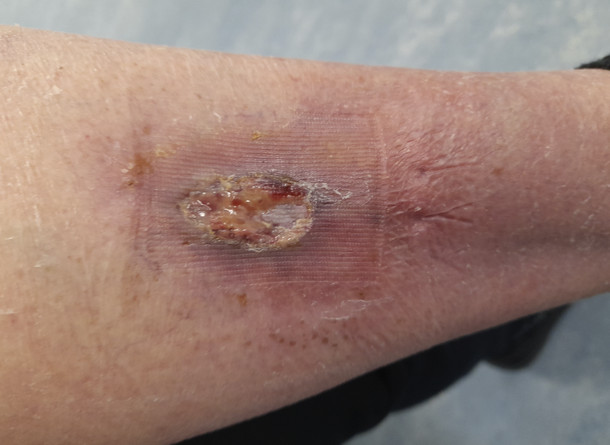
Below is a recent patient with a post surgery wound after a couple of months of NHS treatment. Damaged by the pressure of the dressings, inflamed skin, overly wet and making no progress. In fact the left edge of the wound is expanding due to honey being applied.
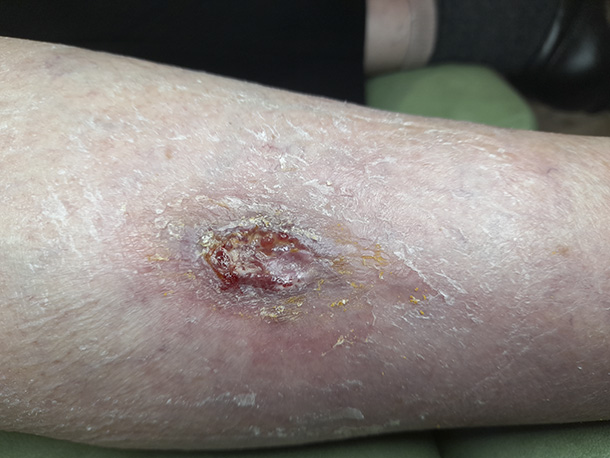
One week after the initial podiatry treatment. After debridement with a scalpel the surrounding skin is looking much happier and the wound is reduced in size.
The following week it is much reduced in size. It is clear that the leg was perfectly capable of healing and it was being held back by the previous dressings.

End of the 3rd week it has nearly healed. If the patient hadn't come to us it is almost certain it would still look the same as the first picture, if not worse. From this point it just needed a dressing to cover but no further treatments.

The next time the patient attended for podiatry, a month later, it was fully healed

Another patient:
 
Above you can see a typical dressing used by the NHS. The skin around the wound is red with inflammation, overly wet and dented where the dressing has applied pressure. This was being treated for months by a hospital outpatient clinic, the protocol is the same whether in a GP surgery or NHS hospital.
Below one week after starting podiatry treatment and the inflammation is nearly gone. The wound scabbed over and after damage free debridement with a scalpel, there is a nice clean wound with a granulating base ready to heal.
Without a scalpel the scab would have been impossible to remove without causing damage but left in place it would have hindered healing. The temptation then would have been to make it very wet again so it could be rubbed off, but that makes the wound too wet again, which delays or prevents healing.
 
The following week it was nicely filled in (below left) and could be left to scab over and heal. A few weeks later the patient reported that the scab had come off and sent a picture of the scarred but perfectly healed leg. Again if they hadn't come to our clinic its almost certain it would have been in the same static situation we found it.
 
What is the cost of private treatment?
This is just standard podiatry work so the cost is the standard £40 an appointment plus the cost price of dressings which for a single ulcer over a few weeks could be an additional £15-25 total. Usually 3 to 4 appointments are enough to heal a superficial wound on a healthy leg, so all in £120 to £160. If you cannot afford this please ring to discuss your case as we might still be able to help.
If there are significant underlying health problems or it has become a deep chronic ulcer it will take longer and unfortunately in rare cases there are some ulcers that might not heal without some other intervention such as surgery on your blood circulation. At the initial assessment estimation of these things can be given and it will be clear if the leg is responding well after a few appointments.
Ideally patients should attend to try podiatry before trying compression bandaging which is increasingly being applied to healthy legs in the NHS.
When allowed to, the body has an amazing ability to heal. A foot or leg that was healthy before an injury usually will heal surprisingly quickly regardless of how bad the ulcer has got, though we're finding legs that have previously had compression bandaging (tight wrapping not just stockings) take a while to recover before they begin to heal.
Some testimonials from previous patients
Wanted to say how pleased I am that you were able to hasten the healing of my leg wound. Following the procedure to remove the carcinoma from my leg at southmead I was having it dressed twice weekly by gp surgery without showing any signs of healing in 6 weeks. After just 3 visits to you it improved and now is nicely healed. Thank you.
Mrs Celia Elvin
____________________________________________________________________________
My elderly friend had an ulcer on her leg for almost two years and was being treated weekly and sometimes twice weekly by local nurses who tried various methods including manuka honey. She also attended Mr. Thomson's podiatry clinic on approximately 6 weekly intervals and on one occasion Mr Thomson noticed her bandage which was loose and he offered to re-dress her leg. Seeing what was being done he suggested an alternative treatment which seemed to help. However on her next visit to the nurses they once again used the honey and it deteriorated again. Finally Mr. Thomson treated her ulcer exclusively and it healed up after just 3 treatments.
Mrs V Maule
____________________________________________________________________________
Due to a few falls I had a wound on the front of one of my legs.
I was back and forth twice a week to the doctors surgery for two months
having nurses dressing it with honey, just making it wetter rather than
drying it out.
Mr Thompson spotted it on one of my foot appointments and asked if he
could take a look. He was concerned at how wet the wound was and redressed it.
Soon the wound showed signs of healing and within three weeks was as
good as new.
Thank you Mr Thompson for all your help.
Sue
____________________________________________________________________________
I started attending Paulton Podiatry Clinic because I had an ulcer that wouldn't heal for over a year. After numerous visits to my GP surgery no one made the link to my pre-existing health conditions (neuropathy) or even diagnosed it as an ulcer. On visiting Paulton Podiatry Clinic, it was immediately identified as an ulcer and I was given the correct dressing as well as really constructive advice on what to do and not to do. I was surprised how contradictory it was to advice I had been given at my GP surgery and it was clear that my ulcer would have never healed properly if at all had I not seen Mr Thomson. After a few visits, the ulcer was fully healed within 5 weeks. This was 8 years ago and thanks to the ongoing care I receive at Paulton Podiatry, the ulcer has never returned.
Attending Paulton Podiatry Clinic regularly has effectively prevented new ulcers and stopped my condition impacting my life - I'm still able to run around after my little girl and for that I'm very grateful!
Mrs K Ring
____________________________________________________________________________
After having cellulitis I was left with abscess on my shin which had to be cut and drained and left me with an open wound. After 8 weeks of appointments at the hospital it was not healing due to the wrong dressings used, so decided to see the podiatrist. Within 1 week the wound had shrunk in size, scabbed over and looked far better. After another appointment it was nearly healed. 5 weeks later the scab came off and it is fully healed so can now have my double knee operation at last. Thanks to Paulton Podiatry.
Mrs Deb Cockram
____________________________________________________________________________
I was aware Mr Thomson treats leg ulcers so when my husband developed one we sought his help. It only needed two appointments and with the right care and advice it has healed in a few weeks. Will certainly seek his help again if concerned.
Mrs Mary Cookson ____________________________________________________________________________
I injured my leg in the garden and was being treated at my surgery twice a week for about 2 months but it wasn't getting any better at all. Mr Thomson offered a different way of treating it and after 1 week it was half the size, and another week it was nearly healed. It only needed those 3 appointments and then it was healed. I highly recommend his service.
Sue Maule
____________________________________________________________________________
MESSAGE FOR REGISTERED NURSES:
If you are a GP practice or registered nurse involved with leg ulcer care please contact the clinic to ask about the free training we offer in podiatry wound care methods, including superficial sharp debridement. |